As part of the standard management for inflammation of the front of the eye, a dilating drop is instilled in the office and is usually prescribed for use at home as well. The purpose of the dilating eye drop is to keep the pupil large to prevent posterior synechiae from forming or to break apart synechiae that are already formed. Having a dilated eye can create light sensitivity and reduce near vision, but will also alleviate much of the pain that comes with eye inflammation.
What is Anterior Uveitis?
Anterior uveitis is the term for inflammation of the front of the eye including the iris (the colored part of the eye) and the ciliary body (the muscle that changes the size of the pupil).
This inflammatory condition will have symptoms including a very red eye, pain, light sensitivity, and blurred vision.
In the most severe cases of anterior uveitis, the iris can become so inflamed that it begins to adhere to the crystalline lens in the eye. When the iris “sticks” to the lens, it is called posterior synechiae.
Concerns with Posterior Synechiae
Posterior synechiae are not an uncommon finding in anterior uveitis, but they do pose a much higher risk for vision than cases of uveitis without synechiae.
The posterior synechiae will restrict the movement of the pupil and cause the pupil to remain fixed due to the adhesions.
This will create difficulties with focusing and adjusting focus, but these are short-term issues that resolve once the synechiae are gone.
The more concerning risk with posterior synechiae is that the adhesion between the iris and the lens will restrict the drainage of fluid from the eye.
This can increase the pressure in the eye and lead to angle closure glaucoma. Angle-closure glaucoma has the risk of permanent vision loss if not treated quickly.
What are Dr. Woo's Thoughts about Posterior Synechiae?
Posterior synechiae is something I see very commonly in patients who have inflammation in their eye (called iritis).
When the fluid in the eye becomes inflamed, it can also become sticky.What happens now is the iris (the colored part of the eye) can start to stick to the front surface of the lens.
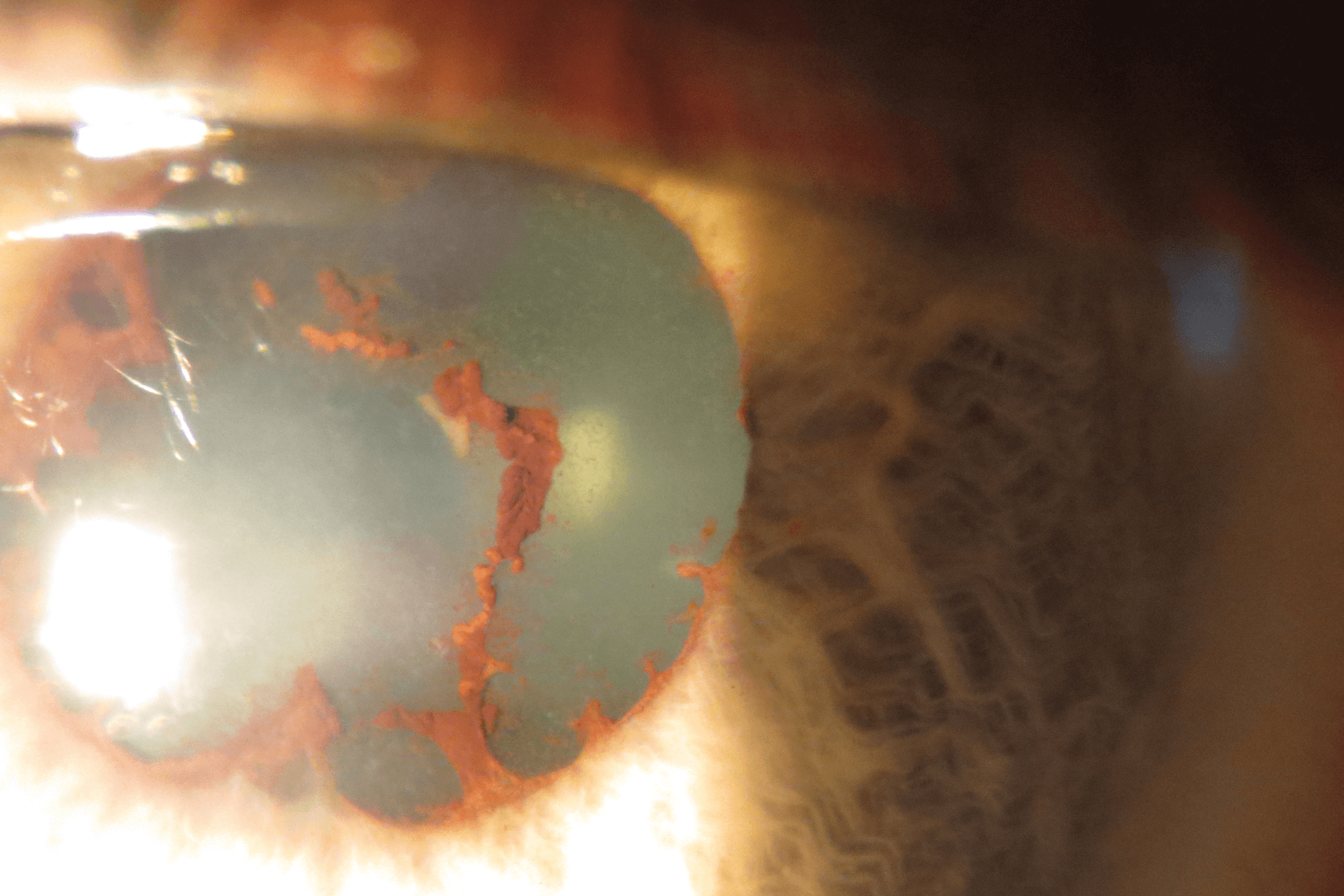
As the pupil dilates and the iris starts to pull away from the stuck part on the lens, small fragments of the iris can be left behind like in this photo.
If iritis or inflammation in the eye is present, your doctor will usually put in a dilating eye drop.
This is to dilate your eye and pull the iris away from the front of the lens so that it can’t get stuck.
I usually use atropine or homatropine, but to get the patient started, I will use cyclopentolate 1% because this is what I have in the office.
Then they can pick up their Rx for the longer lasting eye drop.
If you’ve ever had an inflamed eye and wondered why your doctor dilated your eye, now you know!
Treating Posterior Synechiae
Given the relative urgency and risks associated with posterior synechiae, the treatment of this condition is initiated in the office and then carried over into at-home treatment.
In the office, the eye doctor will attempt to “break” the synechiae by dilating the pupil. When the pupil dilates, the posterior synechiae are pulled apart and the adhesion between the iris and the lens is removed.
If the doctor is able to break the posterior synechiae, two eye drops are usually prescribed for use for a few days before returning for a follow-up. These are a steroid eye drop and a dilating eye drop.
If the posterior synechiae do not break fully, the doctor may elect to have the dilating drop used for a day and then evaluate to determine if the synechiae have broken.
Dilating Drops Used for Posterior Synechiae
The dilating eye drop which is considered the standard for treating posterior synechiae is homatropine.
However, this drop can be difficult to obtain and is rarely found in offices.
In place of homatropine, atropine, cyclopentolate, or phenylephrine may be used to break the posterior synechiae.
Whichever dilating drop is used and prescribed, the goal is to keep the pupil large and prevent the potential for new posterior synechiae to form.