What is Glaucoma?
Glaucoma is one of the leading causes of blindness for older aged individuals. It represents a group of conditions that damage the optic nerve head (the nerve in the back of the eye that is responsible for good clear vision). Although the true mechanism of action of glaucoma is not entirely understood, a high intraocular pressure (IOP) coupled with a weak lamina cribrosa (a supportive collagen structure surrounding the optic nerve) contributes to damage to the optic nerve head. This leads to excavation or loss of optic nerve tissue over time, leaving less and less nerve fibers available to transmit information needed for the visual processing centers of the brain. Vision loss due to glaucoma is very subtle and progresses gradually over time. Therefore, vision loss comes with no warning signs and may not be detected until very late in the disease process. The vision loss from glaucoma is irreversible and limits your field of view, eventually causing a tunnel like effect. Your eye doctor will be able to detect early signs of glaucoma through regular eye exams and help prevent vision loss by initiating treatment. Luckily, with early treatment most patients will not develop severe vision loss with glaucoma.
What are the different types of Glaucoma?
Glaucoma is an umbrella term for many subsets of the condition. Glaucoma can be caused by many things and can be broken down into multiple categories.
- Open angle glaucoma
- Primary open angle glaucoma is the most common type of glaucoma. This type of glaucoma occurs gradually and does not have symptoms until further into the disease process, often occurring without pain or visual changes. The drainage system of the eye does not work as well and becomes clogged like a sink drain. This causes pressure to build inside the eye and presses on the optic nerve to cause irreversible damage. Patients of African American descent and those that are near sighted (myopic) are more at risk of developing open angle glaucoma.
- Angle closure glaucoma
- Angle closure glaucoma is a rapid acute occurring type of glaucoma. In contrast to primary open angle glaucoma, angle closure results in dramatic symptoms at onset. The patient may experience nausea, vomiting, headaches, blurry vision, and eye pain. This condition occurs due to the anatomical makeup of the eye. In these patients, the iris (the colored part of the eye) can become too close to parts of the drainage system and results in a blocked drain. When the angle where fluid drains becomes entirely blocked, the pressure of the eye can rise quite rapidly. Angle closure is a true ocular emergency due to the potential for rapid vision loss. Far sighted or hyperopic patients are more at risk of angle closure. Older age also places you at higher risk of developing angle closure due to changes in anatomy within the eye.
- Normal tension glaucoma
- Normal tension glaucoma describes a population where the intraocular pressure is below 21mmHg (the standardized cut off for glaucoma risk). These patients are thought to develop glaucoma due to blood flow issues. Patients of Japanese descent are more at risk of developing normal tension. This condition is associated with Raynaud's phenomenon, sleep apnea, and hypotension. Vasospastic events have a high correlation factor with this type of glaucoma. The visual field defects in normal tension glaucoma tend to be deeper and closer to one’s central vision than other forms.
- Congenital glaucoma
- Congenital glaucoma can occur in children due to poor eye development. This causes problems with outflow that result in increased eye pressure. These children typically present with excessive tearing of the eyes, blinking, and sensitivity to light. The appearance of their cornea (the front surface of the eye) may appear differently, usually enlarged. This is termed bupthalmos and is characterized by a cornea that is >12mm in diameter due to a rise in pressure in the eye. Early treatment of congenital glaucoma is imperative in order to prevent severe developmental consequences in vision. If left untreated, this can lead to blindness. Treatment usually involves surgery sooner than other forms of glaucoma.
- Plateau iris syndrome
- Plateau iris syndrome is a form of primary angle closure glaucoma. It is caused by a convex peripheral iris that blocks the outflow structure of the eye. This condition can be diagnosed by your eye doctor using special lenses to view the angles of your eyes.
- Secondary glaucoma
- Pigment Dispersion syndrome
- Pigment dispersion syndrome results in glaucoma because pigment cells are released from the iris and become lodged in the drainage system of the eye. This is more common in young myopic (nearsighted) males. The patient may experience transient episodes of blurry vision during exercise. Your eye doctor will use special lenses to evaluate the angles of your eyes to see if there is a pigment present.
- Pseudo exfoliation glaucoma
- Pseudo exfoliation glaucoma results from deposits of fibrillary residue from the lens and iris epithelium within the drainage system of the eye. This condition is more common in Scandinavian populations. A deficiency in folic acid, high altitudes, and increased caffeine intake increase your risk of developing this condition.
- ICE
- Pigment Dispersion syndrome
- Iridocorneal endothelial syndrome results in glaucoma due to developmental abnormalities in the eye. This leads to secondary angle closure from blocking the drainage system. This condition is also associated with iris atrophy, corneal edema, and abnormal pupils.
- Traumatic glaucoma
- Trauma results in angle recession glaucoma by causing damage to the drainage system of the eye. This may occur in association with trauma induced or rosette style cataracts.
- Traumatic glaucoma
- Glaucoma Suspects
- Glaucoma suspects describe patients with ocular hypertension (higher than normal eye pressure) but who do not possess any signs of optic nerve damage. These patients are at a higher risk of glaucoma. These patients are watched more closely than the normal population but do not typically undergo treatment.
What are the symptoms?
The signs and symptoms of glaucoma depend on what type of glaucoma you are diagnosed with. If your glaucoma is acute and has a sudden onset, you may experience severe headache, eye pain, nausea and vomiting, haloes around lights, and blurred vision. However, if your glaucoma is chronic you may experience no symptoms until advanced stages. In these cases, you may experience blind spots in the periphery in both eyes or tunnel vision. If glaucoma is left untreated, the vision loss will progress and eventually lead to blindness.
What tests are used in glaucoma diagnosis?
A patient’s risk and diagnosis of glaucoma is done via multiple tests within a clinical setting. This involves the measurement of the patient’s eye pressure using tonometry. A probe is used to evaluate the pressures within the eye. The standard range of normal IOP is typically between 12-22mmHg. A higher than 22mmHg puts you 2 standard deviations above the national average of 15.5mmHg and therefore put you at higher risk of developing glaucoma. A dilated eye exam is imperative in order to evaluate the optic nerve as this is the place you will see damage from glaucoma. Visual field testing is imperative to determine progression of the disease. Visual field findings are less significant early on in the disease and rapidly progresses in late advanced stages. Imaging tests such as an OCT can help map out the optic nerve and show any areas of tissue loss. Gonioscopy is used to evaluate the angles of the eyes, the drainage site of the eye. Gonioscopy involves specialized lenses that allow your eye doctor to evaluate these structures. Pachymetry describes the measurement of corneal thickness. A thin central corneal thickness puts a patient at higher risk of developing glaucoma due to decreased structural support. All testing done is at no risk to the eye. At most, testing may feel minorly uncomfortable. Dilation may temporarily blur your near vision and make you light sensitive for a few hours. Proper testing and evaluation of the eye is imperative in forming a diagnosis.
What treatment options are available for glaucoma?
Treatment for glaucoma centers around controlling intraocular pressure and keeping it as low as possible in order to prevent further damage to the optic nerve head. There are a myriad of topical eye drops that are used in glaucoma to target IOP. The type of glaucoma drops that a patient is prescribed depends on their personal medical history and risk factors for side effects. Glaucoma is a chronic condition and must be treated indefinitely. Some glaucoma eye drop categories include:
- Prostaglandin analogs
- Prostaglandin analogs are typically the first line treatment for glaucoma. They work to increase outflow of the eye. They have a better dosing schedule than the other drops at once per night. They have a typical IOP lowering ability of about 30-35% of the original IOP which is more effective than most other drops. Prostaglandin analogs cannot be used in patients with a history of uveitis or any other inflammatory condition in the eye. Your eye doctor will be able to determine if this is a suitable drug for you. Some potential side effects of prostaglandin analogs include periorbital skin atrophy, eyelash growth, eye color darkening, and redness of the eyes.
- Carbonic anhydrase inhibitors
- Carbonic anhydrase inhibitors work to decrease aqueous production within the eye, effectively lowering IOP. These drugs are available in oral form as well and are most commonly used in cases of angle closure glaucoma. These drugs can cause rapid decrease in IOP. These drugs are contraindicated in pregnancy, severe COPD, and kidney problems. Some side effects include nausea, vomiting, metallic taste, paresthesia, and metabolic acidosis.
- Beta Blockers
- Beta blockers decrease aqueous production within the eye. These drugs are contraindicated in patients with COPD, asthma, and bradycardia. These drugs can cause side effects such as dyspnea and bronchospasm. These drugs are about effective at lowering IOP by about 25%.
- Cholinergic agonists
- Cholinergic agonists are less commonly used glaucoma drugs due to their wide range of symptoms. These drugs can cause early cataracts, myopic shift, and brow ache. These drugs work by increasing the main drainage side of the eye—the corneoscleral pathway.
- Rho-Kinase inhibitor
- Rho-Kinase inhibitors are a newer class of glaucoma drugs. They work by inhibiting the enzyme responsible for fluid buildup in the eye. Possible side effects include corneal deposits (verticillate) or eye redness.
- Combo drugs
- Some drugs are formulated as combinations of two classes of glaucoma drugs. This is beneficial by targeting multiple mechanisms of increased eye pressure to effectively lower overall IOP.
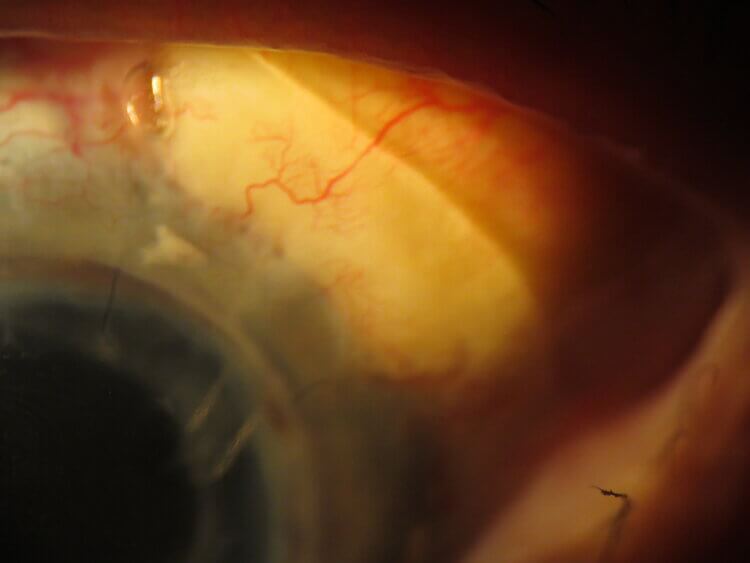
In cases where glaucoma eye drops are ineffectual and optic nerve damage continues to progress, surgical or laser options are considered. Selective laser trabeculoplasty (SLT) or argon laser trabeculoplasty (ALT) are both laser options that focus on the trabecular meshwork of the angle (the main drainage site of the eye). They work to open the drainage site to allow for better outflow. SLT is a newer procedure and is safer overall than ALT. It is also reproducible and can be done multiple times, thereby making this the preferred method over ALT. SLT has similar efficacy to prostaglandin analogs, making this sometimes a first line treatment in cases where patients are not consistent in taking drops. In addition to lasers, surgeries can be performed to place drainage tubes within the eyes to help drain excess fluid.
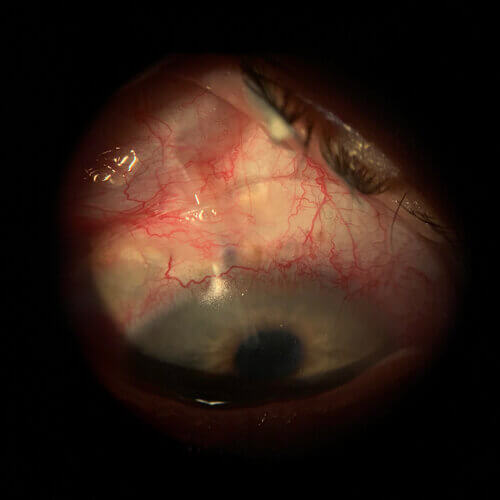
Acute angle closure glaucoma requires different treatment than chronic slow progressing causes of glaucoma. In acute angle closure, a procedure called a “LPI” or laser peripheral iridotomy is performed in order to allow for outflow of the aqueous (fluid in the eye). A laser is used to form small circular holes in the superior part of the iris to allow for outflow. Plateau iris syndrome requires the use of argon laser peripheral iridoplasty (ALPI) instead of LPI. LPI treatments would not be effective in treating plateau iris.
What prevention options are available for glaucoma?
Due to the lack of symptoms in most cases of glaucoma, it is imperative to get regular eye exams. Your eye doctor can help detect glaucoma in the early stages in order to prevent significant damage from occurring. If you are aware of having a family history of glaucoma, more frequent screenings may be required due to the tendency for glaucoma to run in families. Regular exercise can help contribute to lowering IOP. Wear protective eye gear to avoid injuries and further damage to the eye.